More information
I am the Dra. Teresita Pannaci
Specialist in the treatment of craniofacial malformations such as cleft lip and palate (FLP), hemifacial microsomia, the mandibulary disposses, Pierre Robin syndrome, among other congenital conditions.
I welcome you to this space, designed to provide clear and reliable information to families, caregivers and patients living with these conditions. Here you will find guidance on available treatments, the necessary medical follow-up and the support we can offer from day one.

1. CRACKS LABIOPALATIN
1.1 What is a cleft lip and palate??
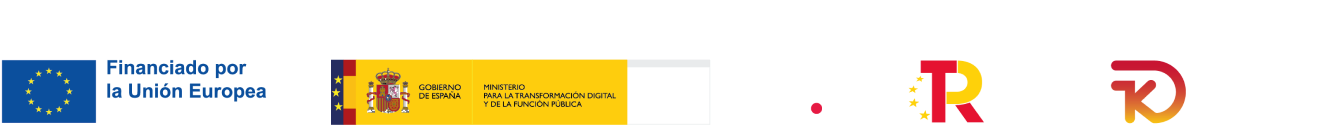
Cleft lip and/or palate are alterations in craniofacial development that occur when certain parts of the face do not join together correctly during the first weeks of pregnancy.. They are also known as congenital craniofacial malformations.. This lack of fusion can affect the upper lip, the palate (the roof of the mouth), or both.
Cleft lip and palate is a congenital craniofacial malformation most common in the human being.
In most cases, clefts of the lip and palate appear isolated, that is to say, without being associated with any other medical condition. However, In certain cases they can be part of a set of alterations known as syndrome, where the fissure is one of several features present.

1.2 Why does a cleft lip and palate occur?, what is the cause?
The exact cause of clefts of the lip and palate is still not known with certainty.. However, The most accepted theory is the multifactor theory, which indicates that this condition may be due to a combination of genetic and environmental factors that act during the first weeks of pregnancy, just when the baby's face and palate are forming.
One of the most studied environmental factors is the low intake of folic acid and B complex vitamins in the mother's diet.. Folic acid is an essential vitamin for the proper development of the nervous system and embryonic tissues.. That's why, It is recommended that women of childbearing age begin taking folic acid at least three months before becoming pregnant., since many times the daily diet does not cover the necessary requirements.
In addition to vitamin deficiency, Maternal stress has been identified as a possible risk factor in the development of cleft lip and palate.. Prolonged stress can alter hormonal balance and negatively affect fetal development.
Other environmental factors that have also been associated include maternal exposure to phosphorus pesticides., polluting or toxic substances, especially during the first weeks of pregnancy. These substances can interfere with the normal processes of formation of facial structures in the embryo..
Taking care of the mother's physical and emotional health before and during pregnancy is a fundamental way to contribute to the healthy development of the baby.. Good nutrition, Medical support and stress reduction can make a big difference.
1.3 Types of cleft lip and palate
Not all cracks are the same. There are different types, depending on which parts of the mouth and face are affected. Next, We explain the most frequent ones:
- lip cleft (lip cleft):
Affects only the upper lip. Can be presented on one side only (unilateral) or on both sides (bilateral). Medical literature indicates that fissures on the left side are more common than those on the right side.. In some cases, the crack is just a small cut; in others, can extend to the nose. - Cleft palate (cleft palate):
Affects only the palate, that is to say, to the roof of the mouth. It can compromise the soft part (closest to the throat), the hard part (most previous) or both. Sometimes, may go unnoticed at first, especially if it is small. - Cleft lip and palate:
It is the most extensive and affects both the upper lip and the palate.. Like the previous ones, can be unilateral or bilateral.
When it is complete, the opening may extend from the lip to the deepest part of the palate.
Each type of fissure requires an individualized treatment approach, and the good news is that there are very effective techniques to help the baby feed better, prepare him for surgery and improve his facial and functional development.

2. OTHER ALTERATIONS IN CRANIOFACIAL DEVELOPMENT
The alterations of craniofacial development are very varied. In some cases, in addition to cleft lip and/or palate, Other structures of the face and skull may be affected, like bones, the muscles, cartilage or soft tissue. some are:
2.1 Hemifacial Microsomia (MHF)
It is a condition in which one side of the jaw (lower jaw) grows less than the other, causing facial asymmetry. This difference may become more evident as the child grows older., since the two sides of the face develop unevenly.
2.2 Disostosis Mandibulofacial (Treacher Collins Syndrome)
It is a genetic disorder that can affect the development of the cheekbones, the jaw, ears and eyelids. Children may present characteristic facial features and, in some cases, hearing loss.
2.3 Pierre Robin Sequence (formerly called Pierre Robin Syndrome)
It is characterized by a small jaw (micrognatia), the tongue in a more posterior position than normal (glosoptosis) y, frequently, cleft palate. This can make feeding and breathing difficult in the first months of life..
2.4 Apert syndrome
Affects both the skull and the hands and feet. Skull bones fuse too soon, which can change the shape of the head and affect brain development. It is common that there are also facial and dental alterations.
2.5 What is a syndrome?
There are many other conditions where craniofacial alterations are part of what is known in medicine as a syndrome..
in medicine, and syndrome It is a set of signs and symptoms that usually appear together and share the same cause., What can a genetic alteration be like?.
When a child presents a fissure or alteration in the face as part of a syndrome, That means there are other structures in the body that may also be compromised., Therefore, medical monitoring requires a more comprehensive and coordinated approach between different specialists..
3.PRENATAL DIAGNOSIS OF Cleft Lip and Palatine
3.1 I am pregnant and they told me that my baby has a fissure.. and now what do I do?
Receiving a prenatal diagnosis of cleft lip and palate can be shocking and generate many emotions.: surprise, fear, doubts. It's normal to feel this way, little by little you will assimilate the information.
In many cases, at the crack can be detected during prenatal check-ups, through a routine ultrasound, especially from the second trimester of pregnancy.
However, It is very important to know that you are not alone. There are specialized medical equipment and resources available to accompany you from pregnancy and help you and your family prepare to receive your baby with all the information and support necessary. Here you have a real image of a baby 26 weeks of gestation and the ultrasound has revealed the fissure on the left side of the lip.
3.2 Next steps…
Once the diagnosis is received, It is advisable to request an appointment specialized prenatal counseling. You can schedule a consultation to receive medical and emotional guidance (It can be online or in person). During this appointment, will be explained clearly:
- What does it consist of? exactly the condition detected.
- That specific care requires pregnancy.
- What will be the first steps at birth.
- What specialists will be part of the team that will care for the baby (surgeon, specialist dentist, pediatrician, speech therapist, etc.).
- If you want, get in touch with other families, facilitate that support network
3.3 Care during pregnancy
In most cases, pregnancy can continue normally. However, There are some general recommendations:
- Maintain a balanced diet and take care of the body as in any pregnancy
- Go to control prenatal regular.
- Avoid stress: he emotional support It is essential.
- Get informed from reliable medical sources, avoiding the overload of poorly verified information on the internet.
- Support network with other families or mothers who are going through the same thing or have already experienced it.
3.4 Breastfeeding and cleft lip and palate
Many mothers wonder if they will be able to breastfeed their babies with clefts.. The answer is: Yeah, In many cases it is possible. However, may require specialized guidance and the use of adapted techniques or devices, especially if the cleft involves the palate.
During prenatal counseling you can also:
- Explain the possibilities of direct or expressed breastfeeding.
- Recommend the option of special bottles.
- Refer to lactation specialists with experience in orofacial clefts.
3.5 Receive your baby with confidence and love
Have information, a plan and a team that accompanies you makes all the difference. Our goal is empower you as a mother or caregiver to make you feel calm and prepared from the first day.

4. SPECIAL CARE of the patient with FLP
4.1 CISS HYGIENE
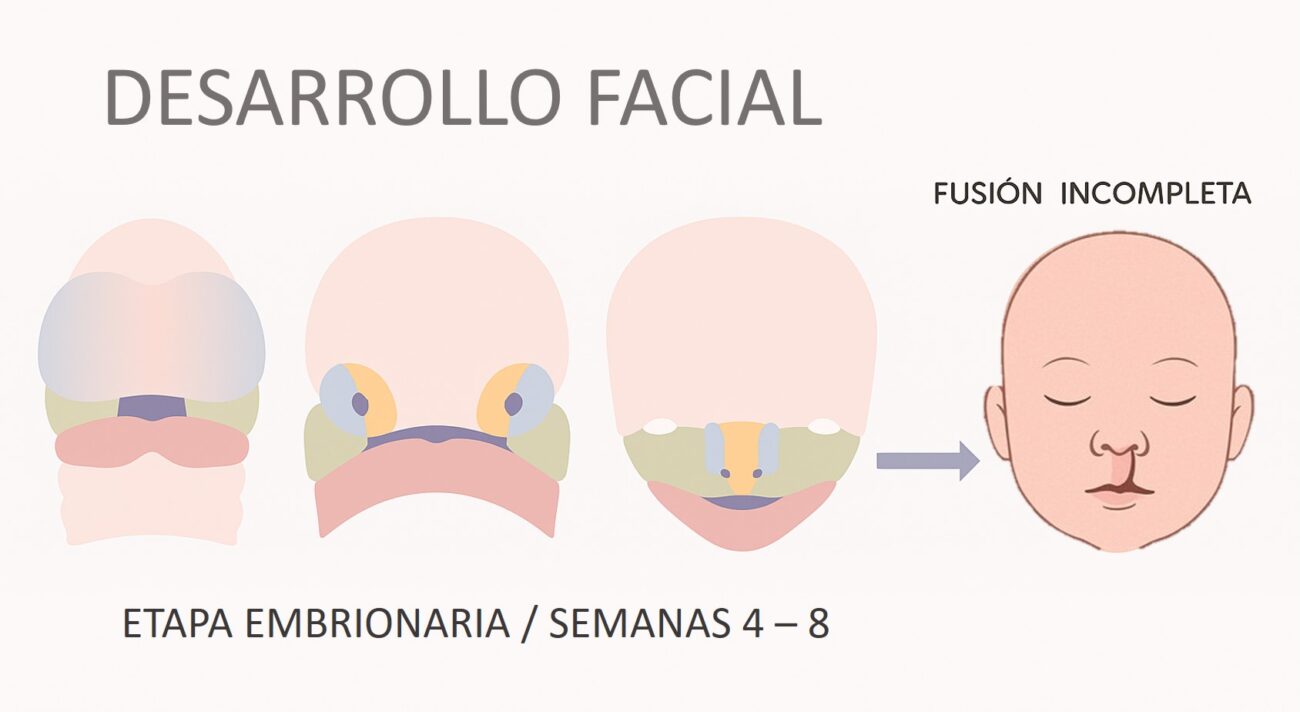
The baby's mouth and nasal cavity should be kept clean and free of milk residue., food or mucus. Due to the fissure, there is a direct communication between the mouth and nose, which makes it easier for milk to pass into the nasal cavity each time the baby feeds. This situation can cause irritation and promote greater mucus production..
Daily hygiene is essential to avoid infections and discomfort. It is recommended to do it twice a day, avoiding doing it right after feeding the baby.
How to clean the baby's mouth?
- Use a clean and preferably sterile gauze, moistened with warm water.
- With very clean hands (or wearing gloves), wrap one finger with the gauze and, very gently, put it in the baby's mouth.
- Make gentle movements to remove traces of milk or food. Don't forget to gently clean the edges of the fissure and the tongue.
And the nose?
- Use another gauze pad slightly moistened with warm water..
- Gently clean the nasal passages from the outside, without inserting swabs or objects into the nose, as this can cause irritation or injury.
Maintaining good oral-nasal hygiene helps the baby breathe better, eat more comfortably and reduce the risk of infections.
4.2 FEEDING
Feeding a baby born with a cleft lip and/or palate can present certain challenges., but with the right guidance and the right resources, it is possible to achieve effective and safe nutrition.
- Direct breastfeeding
The best option whenever possible is breastfeeding. Breast milk is not only the most complete food for your baby., but also strengthens the emotional bond thanks to skin-to-skin contact between mother and child..
However, Some conditions can influence whether this diet is achieved successfully.: baby's position when breastfeeding, suction force, the type and size of the nipple, inter alia. That's why, We recommend that you receive specialized breastfeeding advice to evaluate your case and help you establish an adequate diet from the first days.. - Special bottle feeding
Another very valid option is to feed the baby with a bottle.. Currently there are bottles on the market specially designed to control the flow of milk., facilitating feeding of babies with clefts, especially in cases of cleft palate or in babies with Pierre Robin sequence.
Importance of using the Functional Plate for adequate power
For both direct breastfeeding and bottle feeding, It is essential that the baby uses an intraoral plate (also known as Functional Board). This must be made to measure, preferably in acrylic and with a functional design that adapts comfortably to your palate.
The plate plays the role of an “artificial palate”: allows the tongue to have a firm surface to rest on for safer swallowing, preventing the passage of milk into the nose and reducing the risk of choking. Once the baby is accustomed to his Functional Plate, You can use almost any type of bottle.

4.3 PLATE CARE
The Functional Plate is a device tailored to the baby's palate that is made of acrylic and has a maximum useful life of 3 months, so it should be changed regularly according to your baby's growth.. The Functional Plate must remain in the baby's mouth 24 hours/day. It is suggested to remove it two (2) times a day for cleaning.
How to clean it correctly:
- Wash it under cold running water (never hot).
- Brush gently with a soft-bristled toothbrush.
- Use non-abrasive toothpaste or neutral gel.
Rinse well and place it back in the baby's mouth as soon as possible..

5. MULTIDISCIPLINARY TEAM FOR A COMPREHENSIVE TREATMENT
Learn more
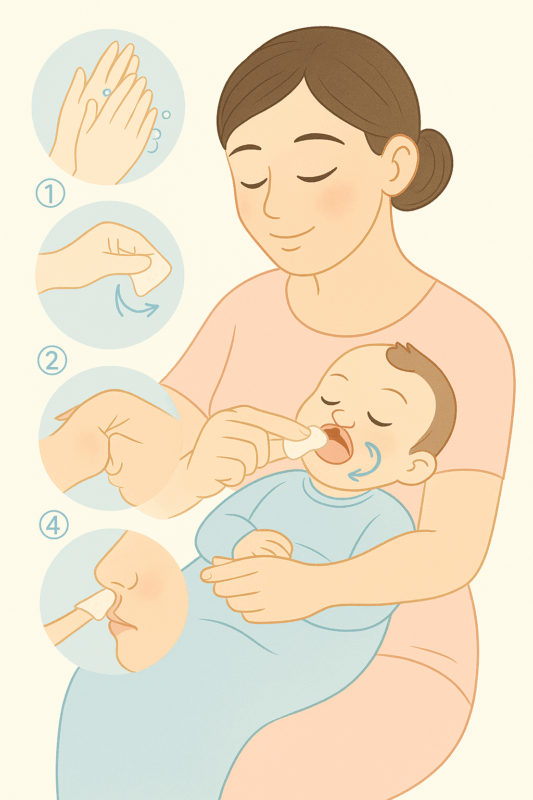
Treatment of a baby with cleft lip and palate involves specialized and coordinated care. Because this condition affects different functions and structures of the face, Its approach requires the participation of a multidisciplinary team.
This team is made up of professionals from different areas of health, who work together to offer the child comprehensive care from birth to full development. And most importantly: The family is also a fundamental part of the team. The accompaniment, Commitment and active participation of parents and caregivers is key to the success of treatment.
The main specialties that make up this team are:
5.1 PLASTIC SURGERY
He is the specialist in charge of performing lip and palate reconstructive surgeries.. Its goal is to improve both the function and appearance of the child's face., helping him to feed, speak and develop appropriately.
5.2 MAXILLOFACIAL SURGERY
Deals with the bony structures of the face and mouth. Your intervention is key when there are alterations in the bones of the maxilla or jaw., especially in complex cases or when corrective surgery is required later.
5.3 PEDIATRICS
This is the doctor who monitors the baby's general growth and development.. Evaluate your health status, monitor your nutrition and vaccines, and coordinates care with other specialists on the team.
5.4 DENTISTRY
Babies with clefts require specialized dental care, if possible, from the day of birth.. Pediatric dentists take care of the child's oral health from the first months. Orthodontists correct the position of the teeth and jaws as the child grows.. Specialists in maxillary functional orthopedics intervene from birth to guide facial growth and help reduce the cleft with custom-made devices, is the preparation before lip and/or palate surgery.
5.5 BREASTFEEDING COUNSELING
Help mothers find the best way to feed their baby, either with direct breastfeeding, expressing milk or using special bottles. Their support is essential to ensure good nutrition from birth..
5.6 Otorhinolaryngology (ORL)
Evaluates and treats ear-related problems, nose and throat. In children with cleft, It is very important to monitor hearing and prevent middle ear infections (otitis), which are frequent due to communication between the mouth and nose.
5.7 LOGOPEDIA
He is the language and speech specialist. Accompany the child throughout their development to encourage good pronunciation, breathing, and speech function, especially after palate surgery.
5.8 PSYCHOLOGY
Provides emotional support to the family and child, helping to face difficult moments of treatment. It also accompanies the child in his social adaptation, school and emotional.
5.9 GENETICIST
Study if the fissure is part of a syndrome or if there is a family history. Perform evaluations to better understand the origin of the malformation and guide the family in future decisions.
5.10 FAMILY UNIT
The family is the most important pillar of treatment. love, The daily care and commitment of parents and caregivers are essential for the success of each step. You are an active part of the team.
6. TREATMENT SEQUENCE CISSED PATIENT

Learn more
Treatment of a baby with cleft lip and palate requires the participation of a team multi-disciplinary, where each specialist works in a coordinated manner and shares the same approach to diagnosis and treatment. This collaboration allows us to offer the patient the best possible care at each stage of their development., with the aim of achieving a complete and functional rehabilitation.
In this section, I will explain to you clearly and step by step what role we play. dentists specializing in orthodontics and maxillary functional orthopedics within the comprehensive treatment of the cleft baby. Our intervention begins from the first days of life and is adapted to the needs of each stage of growth..
If you have questions or need advice, do not hesitate to contact us. We are here to help you.
6.1 Treatment from birth to lip surgery
When a baby is born with a cleft palate, there is a direct communication between the mouth and the nasal cavity. This condition can make feeding difficult from the first days of life. Due to this communication, the baby cannot suck effectively, either from the mother's breast or from the bottle, and many times the food rises towards the nose, causing discomfort, choking and complications swallowing safely. Besides, breathing while feeding may also be more difficult, which generates greater muscular effort and fatigue.
This situation can compromise the baby's proper growth., making it difficult to gain weight and height. For lip and/or palate closure surgery to have the best results, it is necessary to reduce the width of the fissure before the intervention. This promotes better tissue healing and better aesthetic and functional results..
Treatment objectives in this first stage:
- Rehabilitate basic functions such as suction, swallowing and breathing.
- Decrease the width of the crack.
- Shape the palate towards a symmetrical arch shape.
To achieve this, We apply a technique based on Maxillary Functional Orthopedics (OFM), call Fun-PSY, developed by me more than 30 years. This technique consists of the use of a Functional Board, made of rigid acrylic from a personalized impression of the baby's palate. This plate, comfortable and safe, acts as an artificial palate that facilitates feeding, helps bone growth and guides progressive closure of the fissure.
As the baby grows, The plate must be replaced periodically to adapt to anatomical changes and continue to perform its function effectively.
6.2 A design oriented towards clinical teaching
After cheiloplasty (lip surgery), The surgeon will indicate the necessary care for the wound and will schedule you for postoperative check-ups.. If you want additional support, My team and I are available to accompany you in this stage, resolve your doubts and guide you professionally.
6.3 Treatment from lip surgery to palate surgery
Nails 4 a 5 weeks after lip surgery, We resume the use of the Functional Plate. Although the lip will already be closed, the palate remains open and requires attention to promote its development.
During this stage, the Functional Plate continues to be key to allow adequate power, especially when the pediatrician begins to incorporate baby food and soft foods. It also helps the teeth that erupt to do so in a better position and to continue to progressively close the fissure..
The duration of this phase depends on each case, but it is usually maintained until the surgeon indicates that it is time to perform the palatoplasty, generally between 14 y 16 months of life.
6.4 Support after palate surgery
Postoperative care is essential to ensure proper healing and prevent complications.. We invite you to contact us if you need guidance on this stage.
6.5 Post-palatoplasty phase and early childhood
Past 3 a 6 months since palate surgery, We begin with a complete functional assessment. At this stage:
- We evaluate the bite, chewing function and bone development.
- We apply preventive measures to take care of the child's dental health.
- We provide guidance to parents on cavity prevention.
- If malocclusions are detected, We begin early functional orthopedic treatment to guide maxillary growth.
6.6 Treatment in temporary dentition (of 2 a 6 years)
During this stage, temporary teeth begin to erupt (the so-called “baby teeth”). In some patients, deviations in the bite or uneven growth of the jaw may appear.. That's why, It is important to have regular check-ups with the specialist in Maxillary Functional Orthopedics (OFM), who will evaluate the need to place new functional orthopedic devices that guide the growth of the maxillary bone and help maintain the dental arch in good shape.
Objectives at this stage:
- Stimulate proper growth of the jaw
- Correct bite deviations
- Promote correct tongue position and nasal breathing
- Accompany speech development.
6.7 Treatment in mixed dentition (between 6 y 12 years)
At this stage, the child begins to change his baby teeth for permanent teeth. It is a key moment to detect alterations in bone growth and guide the eruption of permanent teeth. Maxillary Functional Orthopedics treatment can be continued or adapted to facilitate the correct placement of the teeth and prepare the mouth for future treatments such as alveolar bone grafting..
Objectives at this stage:
- Guide tooth replacement
Stimulate the growth of the jaw in case of deficiency - Promote a balanced bite
- Prepare the patient for graft surgery if necessary
6.8 Alveolar bone graft (between 8 y 10 years)
Many children with clefts need surgery called an alveolar bone graft., which consists of placing a small fragment of bone in the area of the gum where there is an interruption (at the crack). This is done to strengthen the bone structure of the jaw and allow the permanent canine to (tusk) erupt properly.
The orthodontist or functional orthopedist will be in charge of preparing the space necessary for this surgery..
After the operation, A follow-up is carried out to confirm that the graft has been successful.
6.9 Orthodontic treatment in adolescence
When all the permanent teeth have erupted (usually between 12 and the 14 years), the need for orthodontic treatment with braces or other systems is evaluated. Orthodontics seeks to align the teeth, close residual spaces of the fissure, improve the bite and prepare the patient for possible orthognathic surgery if required later.
Objectives of this phase:
- Align permanent teeth
- Correct bite problems
- Improve dental aesthetics
- Coordinate with the maxillofacial surgery team if necessary
6.10 Long-term follow-up and control in adulthood
The treatment of cleft lip and palate does not end with initial surgeries or orthodontics during adolescence. It is very important that monitoring continues throughout adulthood, as some functional and aesthetic aspects may require additional adjustments or controls over time.
Once facial growth is complete and dental development is completed, It is recommended to carry out periodic reviews with the multidisciplinary team to assess:
- The functionality of the bite and the relationship between the jaws.
- He speaks and the function of the palate in the articulation of language.
- Facial and dental aesthetics, in case the patient wishes to perform complementary treatments.
- emotional well-being and the patient's social adaptation.
In some cases, it may be necessary to consider additional treatments such as:
- Completion or refinement orthodontics.
- Orthognathic surgeries to improve occlusion and facial profile.
- Prosthetic rehabilitation or dental aesthetics if teeth are missing or have anomalies.
Speech therapy evaluations or psychological support.

Our commitment
Our commitment is to accompany you throughout the entire process, offering individualized monitoring adapted to the needs of each stage of life. Remember that the cleft does not define your child: with proper treatment, can be fully developed, with health, security and trust. In adulthood, there are many alternatives for dental treatments if they are necessary., like veneers, prosthesis, implants, etc.