More information
I am the Dra. Teresita Pannaci
Especialist in craniofacial malformations and in the comprehensive treatment of patients with cleft lip and palate (FLP), a condition representing congenital craniofacial anomaly most common in humans. For more than three decades I have dedicated my clinical practice, teaching and research to the functional approach of these malformations, developing personalized therapeutic strategies from birth to adulthood.
I welcome you to this space, this aimed at health professionals involved in the comprehensive approach of patients with cleft lip and palate and other craniofacial malformations. Specially designed for dentists, orthodontists, specialists in maxillary functional orthopedics, oral and plastic surgeons, pediatricians, speech therapists, otolaryngologists, geneticists and other related specialties.
This space has the aim to share updated clinical information, training resources and practical experiences that contribute to coordinated care, based on evidence and patient-centered.
Our commitment as specialists is to strengthen collaboration between specialties, offer useful tools for daily clinical practice and enrich the multidisciplinary approach that these patients require throughout their growth and development..

1. CRACKS LABIOPALATIN
1.1 Cleft Lip and Palatine: a comprehensive vision for the health professional
Cleft lip and palate (FLP) It is one of the most common congenital anomalies andn humans and its incidence varies depending on the ethnic group. The highest prevalence has been reported in people of Asian origin, followed by those of Caucasian origin (at intermediate frequency) y, in lesser proportion, in people of African descent.
Fissures may occur in isolation or as part of a clinical syndrome.. One of the most reported syndromes is Van der Woude syndrome., in which the gene mutation has been identified IRF6 as responsible for both lip and/or palate clefts and the presence of bilateral paramedian dimples on the lower lip.
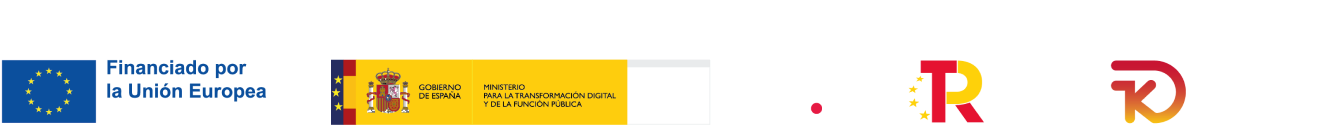
1.2 Origin of the FLP
The formation of the upper lip and palate is a complex process, regulated by genetic factors, molecular signaling pathways and also by environmental influences. This complexity explains the great variability in the phenotypic expression of the cleft.. Critical genes like PAX9, MSX1 and FGFR2 have been described as essential in the normal formation of teeth and other oral structures during the early stages of embryonic development.. Signaling pathways such as WNT, SHH, FGF and BMP participate in cell proliferation and tissue configuration.
Lack of fusion of the upper lip is usually observed unilaterally, most often on the left side, and is slightly more common in men. lip fissures, both unilateral and bilateral, can occur simultaneously with cleft palate.
The use of prenatal ultrasound is a valuable tool for the detection of fetal cleft lip and palate.. Allows the diagnosis of complications associated with craniofacial malformations from early stages. An early diagnosis helps to anticipate the severity of the case and can be useful for the psychological preparation of the family., as well as for adequate planning of the perinatal environment.
1.3 Newborn with FLP
The newborn with cleft lip and palate presents an abnormal communication between the oral cavity and the nasal cavity.. This alteration not only implies a facial defect with aesthetic repercussions., but also a profound affectation of the stomatognathic system and its physiological functions, such as breathing, sucking and swallowing. Consequently, The effectiveness of oral feeding in these infants is considerably reduced., which can compromise weight-height growth, the quality of life and, in severe cases, even life expectancy.
The functional and aesthetic impact of FLP requires early and coordinated intervention by specialized interdisciplinary teams., with a patient-centered approach and based on updated scientific evidence.
The clinical classifications of lip and palate clefts allow unifying diagnostic criteria and guiding treatment in a consistent manner among professionals.. Various systems have been proposed over time., the most used being that of Veau, that groups the fissures according to the extent of the compromised palate; and Kernahan's, which uses a “Y”-shaped diagram to graphically represent the location and severity of the crack. These classifications facilitate interdisciplinary communication and surgical and orthodontic planning..

2. OTHER ALTERATIONS IN CRANIOFACIAL DEVELOPMENT
Craniofacial malformations comprise a wide spectrum of congenital conditions that affect the morphogenesis of structures derived from the first and second branchial arches., including bones, cartilage, muscles and soft tissues of the face and skull. These anomalies can occur in isolation or associated with a cleft lip and palate., which increases diagnostic and therapeutic complexity.
There are also clearly defined genetic syndromes that include clefting as part of their clinical phenotype.. The early identification of these conditions and their correct syndromic diagnosis are essential to establish a comprehensive and multidisciplinary approach., that considers both the functional and aesthetic needs of the patient. Below we will mention the conditions and syndromes associated with cleft lip and palate..
2.1 Pierre Robin Sequence (formerly called Pierre Robin Syndrome):
The Pierre Robin Sequence (SPR) It is a congenital condition that manifests from birth and is characterized by the clinical triad composed of micrognatia (abnormally small jaw), glosoptosis (descent and retroposition of the tongue) y cleft palate of arched and elevated morphology. This combination of alterations significantly compromises the vital functions of the newborn., especially the breathing, suction y swallowing, due to the reduction of the pharyngeal space and, therefore, of the upper airway.
Etiology: There are different theories about the origin of this sequence.. One of the most accepted suggests that glossoptosis—a product of severe micrognathia—prevents the elevation and union of the palatal prominences during fetal development., what gives rise to the cleft palate. However, Other authors propose a primary etiology of genetic or metabolic basis., with alterations in mandibular embryogenesis that occur around the 51st to 6th week of gestation, which secondarily triggers the abnormal position of the tongue and interruption in the fusion of the palate.
Incidence: The Pierre Robin Sequence has an estimated incidence of 1 for each 8.500 live births, although it may vary slightly depending on the population studied.
Diagnosis: The clinical diagnosis is usually established at birth, during physical evaluation of the newborn. Nevertheless, Using high-resolution ultrasonography, it is possible to suspect this condition based on the week 13 gestation, although prenatal confirmation can be complex due to the difficulty in obtaining clear images of the facial region..
Clinical features
- Palatal fissure configuration in “U” shape, in contrast to the “V” characteristic of isolated cleft palates.
- Presence of lingual retroposition and mandibular retrusion evident from the first days of life.
- Functional compromise of the upper airway and swallowing.
Common complications
- Respiratory obstruction, particularly during sleep.
- Difficulties with oral feeding.
- Choking episodes.
- Hypoxemia secondary to partial airway obstruction.
2.2 Hemifacial Microsomia (MHF):
Hemifacial microsomia (MHF) It is a congenital craniofacial anomaly with predominantly unilateral presentation., with an estimated incidence in the United States of 1 each 5.642 births. This condition is considered to result from a vascular accident that occurred during the first weeks of embryonic development., mainly affecting the first and second branchial arches. Therefore, It is included within the spectrum of first and second branchial arch syndromes..
Clinical features: HFM manifests itself with different degrees of regional hypoplasia that involves the temporomandibular and pterygomaxillary regions., affecting both skeletal and neuromuscular structures. The most characteristic alteration is mandibular hypoplasia on the affected side., in which the mandibular ramus may be shortened or practically absent. All patients present some degree of condylar anomaly., which constitutes a pathognomonic sign of this malformation.
As the patient grows, facial asymmetry becomes more evident, progressing in relation to bone development. In a small percentage of cases, hemifacial microsomia can also be associated with cleft palate.
SYNDROMES ASSOCIATED WITH CLEFT LIP AND PALATE
2.3 Sindrome de Van der Woude (Cleft Lip Syndrome with Paramedian Lip Fistulas)
Van der Woude syndrome is one of the most frequent forms of syndrome associated with cleft lip and palate., representing approximately 2% of all orofacial cleft cases. It is characterized by the combination of lip and/or palate cleft with the presence of paramedian lip fistulas., which are small, symmetrically located depressions or dimples on the lower lip.
This disorder is of genetic origin and is transmitted in an autosomal dominant pattern.. Its most common cause is a mutation in the IRF6 gene. (interferon regulatory factor 6), located on the chromosome 1. The penetrance of the syndrome is high, but its expressiveness is variable, which means that there may be members of the same family with very different clinical manifestations, from isolated lip dimples to complete clefts of the lip and palate.
Most frequent clinical characteristics
- Fistulas or paramedian depressions in the lower lip, present in more than 80% of cases. They can be small and asymptomatic, or secrete a slight amount of mucous fluid.
- Furupy and palatina, which can be unilateral or bilateral, complete or incomplete. It may affect only the palate or occur together with a cleft lip..
- Dental anomalies, like supernumerary teeth, hypodontia (especially upper lateral incisors), or teeth with abnormal morphology.
- In some cases, anodontia and enamel alterations have been described.
- Although it is less common, micrognathia may also occur, hypoplasia of the jaw or alterations in the temporomandibular joint (ATM).
Functional and genetic considerations: The diagnosis of Van der Woude syndrome must include a genetic evaluation, since up to 30-50% of cases have a family history, and there is a high risk of recurrence in offspring if one of the parents is affected, even if the clinical manifestations are mild.
From the functional point of view, the presence of cleft lip and palate may require sequential surgical intervention, as well as orthodontic treatments, speech therapy and functional rehabilitation. Early detection of lip fistulas, even without crack, may be key to early diagnosis in family members.
2.4 Treacher Collins Syndrome (Disostosis Mandibulofacial / Franceschetti-Klein syndrome)
Treacher Collins syndrome is a congenital craniofacial malformation, rara, genetically based, whose incidence is estimated to be approximately 2 decade 100.000 births. It is mainly caused by mutations in the TCOF1 gene., although mutations have also been identified in the POLR1C and POLR1D genes. These genetic alterations interrupt the proper development of the structures derived from the first gill arches., bilaterally affecting facial morphogenesis during embryonic life.
The transmission of this syndrome is autosomal dominant., with a penetration close to 90% and variable expressiveness, which explains the diversity in clinical presentation among affected individuals. Some bibliographic sources relate it to chromosome 5q mutations., that interfere with the correct formation of the bones of the skull, cheekbones and jaw. This results in mandibular hypoplasia and retrognathia., that usually evolve into an Angle Class II malocclusion. Besides, This syndrome may be associated with cleft palate, which reinforces its relevance in the context of craniofacial anomalies accompanied by cleft lip and palate..
Most frequent clinical characteristics
- Malformations of the pinna, from its anomalous implantation to microtia or anotia.
- In severe cases, atresia of the external auditory canal and malformations of the ossicular chain may be observed, which leads to conductive hearing loss.
- Bilateral hypoplasia of the malar bones and infraorbital rim, which results in underdeveloped cheekbones.
- Palpebral fissures with antimongoloid obliquity.
- Changes in the lower eyelids, like coloboma and, in some cases, absence of eyelashes.
- Palatine cleft present in a significant percentage of cases.
Common complications
- Respiratory and feeding difficulties during the first years of life, due to narrowing of the upper airways.
- Complex disorders of the temporomandibular joint (ATM), which can lead to malocclusions such as anterior open bite or posterior crossbite.
2.5 EEC syndrome (Ectrodactyly – Ectodermal Dysplasia – Cleft Lip and Palate)
EEC syndrome was first described in 1970 by Rüdiger. It is a rare genetic disorder, characterized by the association of three cardinal signs: ectrodactilia (congenital malformation affecting hands and feet), ectodermal dysplasia y lip-palate cleft. Its inheritance is typically autosomal dominant., although in some cases neomutations can be observed, that is to say, mutations that appear for the first time in an individual without a family history, originating in a germ cell of the parents or in the zygote.
The pathogenesis of this syndrome is not completely clarified., but it has been associated with alterations in the long arm of the chromosome 7, that affect genes expressed in tissues derived from the ectoderm. The ectoderm, one of the three embryonic layers, gives rise to structures such as the epidermis, tooth enamel, sweat glands, hair and nails, Therefore, its alterations explain the characteristic clinical manifestations of EEC..
Most frequent clinical characteristics
- Cleft lip and palate present in approximately 75% of cases. It can be unilateral or bilateral, and affect the lip, the alveolar ridge and the palate in its entirety.
- Ectodermal dysplasia, always present, with demonstrations like:
- Dry and thin skin, often with hypohidrosis or partial anhidrosis (decreased sweating).
- Sparse hair, fragile and clear, due to reduction of melanin.
- Dystrophic nails, hypoplastic or absent.
- Hypoplasia or atresia of the tear duct and decreased tear secretion, which can cause eye discomfort.
Dental alterations:
- Enamel defects, like hypoplasia, hypomineralization or hypocalcification, both temporary and permanent teeth.
- Anomalies in the number and shape of teeth in both dentitions.
Dental considerations
Given the structural involvement of the enamel, Patients with EEC have a high risk of dental caries. Therefore, It is essential to include both the patient and their family environment in intensive prevention programs, with educational focus, fluoridation, regular check-ups and reinforced oral hygiene habits from early stages.
2.6 Apert syndrome (Acrocephalosyndactyly type I)
Apert syndrome is a rare congenital malformation, included within acrocephalosyndactyly, and is characterized by premature fusion of cranial sutures (craniosynostosis), accompanied by syndactyly of hands and feet and, in many cases, cleft palate. Its prevalence is estimated at 1 decade 65.000 a 160.000 births.
This syndrome is caused by mutations in the FGFR2 gene. (fibroblast growth factor receptor type 2), located on the chromosome 10. These mutations affect the development of the skull, face and extremities. Inheritance is autosomal dominant, although most cases occur sporadically, most frequently associated with elderly parents.
Most frequent clinical characteristics
- Craniosynostosis: premature closure of the coronal suture, which causes an acrocephalic or tower-shaped skull.
- Middle facial dysplasia:
- Hypoplasia of the midface.
- Maxillary hypoplasia with relative protrusion of the mandible (pseudoprognatismo).
- Beak-shaped nose.
- Ogival or cleft palate.
- Cleft palate, present in a considerable percentage of cases, may contribute to functional alterations in speech and swallowing.
- Complex and symmetrical syndactyly of hands and feet, with bone and skin fusion of the fingers.
- Exophthalmos (prominent eyes), due to shallow and shallow orbits.
- Delay in psychomotor development, variable intensity, associated with elevated intracranial pressure and brain malformations.
Respiratory and sleep problems, related to facial hypoplasia and upper airway narrowing.
Functional and dental considerations: Maxillary hypoplasia and cleft palate contribute to the presence of severe malocclusions, such as skeletal Class III and anterior open bite. Besides, there may be alterations in tooth eruption, severe crowding, and predisposition to periodontal diseases. The dental approach must be part of a multidisciplinary and comprehensive approach, including craniofacial surgery, orthodontics, speech therapy and functional rehabilitation, from the first stages of life.
2.7 Crouzon syndrome (Craniofacial Dysostosis)
Crouzon syndrome is a syndromic craniosynostosis characterized by the premature closure of one or more sutures of the skull., which affects the normal growth of the skull and face. Unlike other syndromes related to craniosynostosis, Crouzon syndrome is not associated with limb malformations. Its prevalence is estimated between 1 for each 25.000 a 50.000 births.
This condition is due to mutations in the FGFR2 gene. (fibroblast growth factor receptor type 2), located on the chromosome 10. Inheritance is autosomal dominant, although in many cases the mutation can appear de novo. These alterations affect the development of bones derived from the craniofacial mesenchyme., which explains the mainly bone and facial involvement.
Most frequent clinical characteristics
- Premature closure of cranial sutures (especially the coronal), which causes brachycephalic or tower-shaped skull (acrocephaly).
- Hypoplasia of the midface, with retrusion of the upper jaw.
- Exophthalmos (prominent eyes), due to shallow and shallow orbits, with risk of corneal exposure.
- Hypertelorism (increased distance between the eyes).
- Pointed nose and narrow nasal base.
- Relative mandibular prognathism as a consequence of maxillary hypoplasia.
- In some cases, cleft palate or alterations in the palate (pointed palate).
- Recurrent hearing problems, usually due to serous otitis media secondary to Eustachian tube dysfunction.
Functional and therapeutic considerations
Crouzon syndrome can significantly affect facial development, dental occlusion, breathing and vision. Maxillary hypoplasia frequently leads to Class III malocclusion and, in many cases, obstructive sleep apnea due to facial retrusion and upper airway narrowing.
Treatment should be multidisciplinary and begin in the first years of life.. Includes craniofacial surgeries to correct craniosynostosis and prevent increased intracranial pressure, as well as orthognathic surgery, orthodontics, speech therapy and ophthalmological and otorhinolaryngological follow-up.
2.8 22q11 syndrome (22q11.2 deletion syndrome / Velocardiofacial syndrome / DiGeorge syndrome)
22q11 syndrome is a genetic disorder caused by a microdeletion in the long arm of the chromosome. 22, in the region q11.2. It is one of the most common microdeletions in humans., with an estimated incidence of 1 for each 4.000 live births. This condition presents great phenotypic variability, so it can manifest with a very wide spectrum of signs and symptoms, from mild forms to complex multisystem involvement.
This microdeletion affects genes essential for the embryonic development of multiple structures derived from the neural crest mesenchyme., particularly in the facial area, heart and palate. Although most cases occur sporadically, the inheritance pattern is autosomal dominant, and the risk of recurrence in offspring is 50% if one of the parents is a carrier.
Most frequent clinical characteristics
- Cleft palate, present in approximately 70% of cases. May manifest as cleft palate, velopharyngeal insufficiency or submucosal palate.
- Congenital heart defects, especially those related to the outflow tract (as tetralogy of Fallot, common truncus arteriosus or interruption of the aortic arch).
- Characteristic facial features: wide nasal root, prominent nose with bulbous tip, thin lips, low set ears.
- Delayed speech and language development, as well as learning and neurodevelopmental difficulties.
- Variable immunodeficiency, associated with hypoplasia or absence of the thymus.
- Hypocalcemia, secondary to hypoplasia of the parathyroid glands.
- Psychiatric disorders in adolescence or adulthood, like anxiety, mood disorders or schizophrenia.
Functional and therapeutic considerations
Cleft palate and velopharyngeal insufficiency are key manifestations of 22q11 syndrome, and require early evaluation by the craniofacial surgery and speech therapy team. Hypoplasia of the soft palate can cause severe hypernasality, even in the absence of visible crack, making it difficult to acquire intelligible speech.
The management of this syndrome is multidisciplinary and individualized., and includes cardiology, immunology, endocrinology, clinical genetics, plastic surgery, orthodontics, psychology and speech therapy. Molecular genetic diagnosis using FISH or array-CGH is essential to confirm the microdeletion and adequately advise the family..
3.FUNCTIONAL ORTHOPEDIC OF THE MAXILLARIES (OFM)
A therapeutic approach focused on the function and integral development of the orofacial system
Functional Orthopedics of the Jaws (OFM) It is a specialty of dentistry aimed at preventing and correcting dysfunctions of the stomatognathic system., as well as the morphofunctional alterations that derive from said dysfunctions. His therapeutic approach is not limited to aligning teeth, but rather acts on the functional mechanisms that directly influence the growth and development of the jaws and other facial structures..
3.1 a little history
The origins of the OFM date back to 1881, when dr. Jean-Louis Roux, french dental surgeon, proposed for the first time that orthopedic treatment could influence facial bone development through functional modification. Roux was the author of the Theory of Functional Adaptation, which states that the shape of bones can be modified in response to the functional forces that act on them. This pioneering vision made Roux the precursor of Functional Orthopedics of the Jaws..
Later, in 1936, Danish dentist Dr. Viggo Andresen and the German surgeon Dr. Karl Häupl formalized the concept of “functional orthopedics”, focusing their treatments on the rehabilitation of oral functions and muscle stimulation as a way to guide bone growth. This approach supports the principle that adequate orofacial functions, to be restored or stimulated, can correct facial growth vectors.
In contemporary words, Functional adaptation is recognized as the biological principle on which OFM is based. This discipline is based on biomechanics that respects and reproduces natural growth patterns., using gentle forces, biological and directed.
The stomatognathic system: structure and function
When we talk about OFM, we inevitably refer to two key concepts: stomatognathic system and function. This system is made up of all the organs and tissues that are involved in vital functions such as: chew, swallow, talk, pronounce, breathe, smile, kiss and, in the case of neonates, suck. Includes muscles, bones, joints, teeth, language, lips, gums, mucous membranes and glands.
A comprehensive definition of OFM
Dr.. Wilma Simões, international reference in this specialty, defines Functional Orthopedics of the Maxillae as:
“The specialty that diagnoses, prevents, controls and treats growth and development problems that affect the dental arches and their bases, in both the ontogenetic and post-ontogenetic periods, not always through devices but when they become necessary, require for your selection, construction and clinical management: specific diagnostic methods for the multiple possibilities of therapeutic posture change, the use of own anchoring systems, acting in a peculiar way on the teeth (…) and interfere with mandibular dynamics, as well as in the muscular, facial and bone.”
Neuro-Occlusal Rehabilitation (RNO): a complementary vision
Neuro-Occlusal Rehabilitation is part of this same functional approach. (RNO), a theory developed by Dr. Pedro Planas Casanova in 1962. This vision proposes an early intervention to prevent and treat dysfunctions of functional origin that affect the chewing system., and that can lead to dental malocclusions, periodontal alterations and craniomandibular disorders. ElDr. Plan, originally from Barcelona, became one of the pillars of functional thinking in modern dentistry.
Both schools—Simões and Planas—converge on the same therapeutic objective: preserve and restore orofacial functions, activating the muscles involved in chewing, swallowing, phonation and breathing as part of the treatment.
3.2 What forces does the OFM use??
OFM takes advantage of the physiological forces of the body itself, generated mainly by the muscles involved in chewing, swallowing and phonation. These forces are transmitted through specially designed orthopedic devices that act as a functional interface, stimulating bone growth and tissue remodeling.
Roux's principle of Functional Adaptation establishes that there is a direct relationship between form and function: Modified functional loads are capable of causing changes in the internal and external architecture of the bone. In this sense, OFM is based on biomechanics that respects natural development, guiding structures towards more harmonious and functional growth patterns.
3.3 Scope of OFM in the treatment of cleft lip and palate
Application of Functional Orthopedics of the Maxillae (OFM) in the treatment of cleft lip and palate
The use of Functional Plates to support facial growth
Treatment with Functional Plates in infants with cleft lip and palate (FLP) represents a highly effective therapeutic tool, that complements and optimizes the results of reconstructive plastic surgery. These plates allow the upper maxillary arch to be modeled, progressively reducing the width of the alveolar and palatal gap. By achieving a more symmetrical shape of the maxillary arch, better support is provided to the lip, which favors both the aesthetic and functional results after cheiloplasty (lip surgery).
Treatment should continue after cheiloplasty, until preparing the patient for the next surgical intervention: palatoplasty (palate surgery). When a wide maxillary arch is achieved, symmetrical and with a significantly reduced crack, the chances of surgical success are significantly increased.
3.4 When to start treatment with Functional Plates?
Treatment can start from the first day of life of the newborn with FLP. Early intervention offers the best results, since it takes advantage of the potential for growth and plasticity of tissues in the first months. From the first consultation, It is essential to perform a comprehensive evaluation of the stomatognathic system, especially the functional symmetry of the tongue, within a systematized multidisciplinary approach.
3.5 Objectives of treatment with Functional Plates
As has been pointed out, The main objective of OFM is to guide bone growth through targeted functional stimuli. In the context of the FLP, This results in shaping the upper maxillary arch towards a symmetrical “U” shape., reducing the alveolar and palatal gap and preparing the patient for surgical interventions.
Specific objectives in the presurgical phase of cheiloplasty:
- Restore altered orofacial functions.
- Guide the growth of the maxillary segments towards a symmetrical shape.
- Promote mandibular postural change by controlling lingual positioning.
- Increase maxillary dimensions in height, sagittal and transverse direction.
- Decrease the width of the alveolar and palatine fissure both antero-posteriorly and transversely.
- Achieve a harmonious and symmetrical configuration of the upper arch in the shape of a “U”.
- Provide adequate support to the lip to optimize the aesthetic and functional result of cheiloplasty.
Objectives in the presurgical phase of palatoplasty:
- Establish an adequate relationship between the upper and lower jaw, with special attention to achieving the DA (touch between the upper and lower incisors in their incisal thirds), as proposed by Dr.. Wilma Simões.
- Promote the approach between the maxillary segments to allow the natural eruption of the lateral incisors, ideally without the need for bone grafts.
- Maintain DA and eliminate interferences that impede functional jaw movements.
Achieve facial harmony through balanced intermaxillary development.
3.6 Advantages of using Functional Plates
The use of Functional Plates in patients with FLP provides multiple clinical and functional benefits:
- Effectively separates the nasal cavity from the oral cavity.
- Prevents lingual interposition between the maxillary segments.
- Provides a support point for the language, facilitating the suction of food.
- Promotes swallowing, avoiding compensatory use of accessory muscles.
- Reduces the risk of food entering the nasal cavity.
- Stimulates transverse and sagittal growth of the maxillary segments.
- Provides security and peace of mind for parents, by facilitating feeding and supporting the integral development of the infant.
3.7 How does the technique work in patients with cleft lip and palate??
The Functional Plate as an active stimulator of growth and function
The application of the Functional Orthopedics of the Jaws (OFM) in patients with lip-palate cleft (FLP) has proven to be highly effective in accompanying bone growth and rehabilitating orofacial functions.. Although some cases progress more rapidly than others, This is mainly due to individual variability in growth peaks., since treatment begins in infants or newborns, in a stage of high development potential.
As Petrovic points out, cited by Dr.. Wilma Simões, The effectiveness of functional treatment is directly related to the auxological category of the patient: the greater biological growth potential, the greater the tissue response to the stimulation provided by the functional devices. In other words, Bone growth can be guided more efficiently by taking advantage of the active biological windows of childhood development..
3.8 Bone response to functional stimulus
Bone is a dynamic tissue and its response depends on the type of stimulus received.:
- Under tension, bone formation or apposition may occur.
- Under pressure, bone resorption can be induced.
Treatment with Functional Plate does not only pursue structural correction, but his main objective is functional, promoting the restitution of physiological patterns, especially those related to breathing, sucking and swallowing.
The language: biological motor of the Functional Plate
He active element that drives the functioning of the Functional Plate is the tongue. Every time the infant swallows (between 1.500 y 2.400 times a day), the tongue rises naturally and makes contact with the top of the Functional Plate. This, in turn, transmits force to specific areas of the palatal mucosa, previously determined during clinical planning and waxing of the plaster model.
This cycle of repeated stimulation generates biomechanical microloads that activate key points of the palatal mucosa., promoting an adaptive osteogenic response. When the swallowing reflex ends, the tongue descends and the plate interrupts its action, until the next move. This cyclic process allows the treatment to develop continuously and physiologically while the device is in the mouth..
3.9 Factors that may affect treatment success
Possible failures in the results of treatment with Functional Plate may be associated with multiple factors., between them:
- Incorrect design of the Functional Plate or defects in the planning of the wax-up on the plaster model.
- Improper selection of materials or technical errors during the acrylizing process.
- Systemic patient conditions that affect bone growth.
- Nutritional deficiencies, especially in cases where food intake is compromised.
Inconsistent or inappropriate handling of the device by the treating team or caregivers.
Therefore, The success of the treatment requires not only precise technical planning, but also constant and personalized clinical monitoring, as well as close collaboration with parents or caregivers.
4. What is the Pannaci Modification?
A therapeutic strategy to enhance lingual stimulation and bone development in patients with cleft lip and palate
The Pannaci Modification, first published in 1997, It is a technical adaptation applied to the Functional Board used in the functional orthopedic treatment of patients with lip-palate cleft (FLP). This modification aims increase proprioceptive stimulation of the tongue, optimize the adaptive bone response and favor the reduction of the alveolar and palatal gap in the pre-surgical phases.
What does the modification consist of??
The technique consists of making transverse grooves or grooves, parallel to each other and separated by approximately 1 mm, on the acrylic surface of the Functional Plate, on the side of the fissure and located as anteriorly as possible. These grooves provide a differentiated texture that acts as a specific stimulus area for the tongue..
The grooves are made using a metal milling cutter with a cylindrical shape and a flat end., applied by micro-motor or handpiece at low speed. The depth of each spline must be carefully controlled, without exceeding one third of the total thickness of the plate (approximately 1,5 a 2 mm).

Therapeutic rationale and purpose
The language, in its natural swallowing function, actively seeks contact with these stretch marks. This repeated contact enhances sensory and motor stimulation, which generates an increase in the frequency and quality of lingual collisions against the smaller maxillary segment (the one with the least bone development). This action produces an increase in the mechanical load on the bone., which results in an adaptive growth response, expected in the three planes of space: transversal, sagittal and vertical.
This process contributes significantly to:
- Increase in volume of the maxillary segments.
- The progressive decrease in the width of the alveolar and palatine fissure.
- The symmetrical conformation of the upper maxillary arch in the shape of a “U”.
- Optimal patient preparation for cheiloplasty, facilitating a more stable and favorable anatomical base.
Origin and clinical evolution
Initially, This modification was conceived to compensate for the functional deficit of the hemilingual, identified in some patients with FLP during the decade of 1990. Based on the clinical follow-up of patients treated with this strategy, a significant improvement was observed in bone and functional response. As a result, It was established as a clinical protocol to perform the striae from the first plate, regardless of the type or severity of the crack.

5. RESEARCH AND PUBLICATIONS
Three decades of scientific commitment to cleft lip and palate and craniofacial malformations
For more than thirty years, I have dedicated my clinical practice, teaching and research on the functional approach to cleft lip and palate (FLP) and other craniofacial malformations, with an integrative vision that goes from birth to adulthood. along this road, I have developed personalized therapeutic strategies, based on principles of Functional Orthopedics of the Maxillae (OFM) and the need to provide solid scientific support for each of the clinical procedures that we apply to our patients..

Beginnings: Caracas, years 90
My first clinical research experiences date back to the 1990s. 1990, during my work at the San Juan de Dios Hospital in Caracas (Venezuela). There I developed, I documented and published in 1997 the technique known as “Pannaci Modification”, a pioneering advance in the design of Functional Plates for infants with FLP. This technique, today used in various clinical contexts, arose from the functional observation of the tongue in newborn patients with cleft, and the need to adequately stimulate their neuromuscular and bone development from the first days of life.
Collaboration with biomechanical engineering
From 2009 I started a joint line of work with biomechanical engineers, which allowed the integration of new functional and structural analysis methodologies applied to the fissure field.. I have collaborated in advising a degree thesis in mechanical engineering, exploring everything from load modeling on the maxillary bone to functional studies with infants.
One of these works was particularly innovative: We measured the lingual pressure force exerted by babies of 0 a 6 months on the Functional Plate and its grooves, obtaining quantitative data on the stimulus pattern generated during swallowing. This research, currently in publication process, will provide objective and quantifiable evidence on the functional effectiveness of the plate design in neonates.
Research activity in Spain
Since the year 2018, I reside in Spain, where I worked as Senior Researcher at the Vall d’Hebron Research Institute (HIR) in the cleft lip and palate area. In parallel, I provided clinical advice in the Children's Maxillofacial Surgery Service of the Vall d'Hebron University Hospital, until the year 2022.
During this period, I presented and developed two clinical research projects with cleft patients, both approved by the Ethics Committee of the Vall d’Hebron Hospital in 2018 y 2019. These studies are currently in the final phase of analysis and writing., and will be published soon. Its content represents a significant advance in the scientific validation of the functional foundations of OFM applied to cleft lip and palate..
Continuity and training of new researchers
My research activity continues today, both in Spain and in Latin America. I collaborate as a master's thesis advisor in dentistry (TFM) at universities in Europe and America, and I maintain the line of interdisciplinary research with the International University of Valencia, particularly in projects aimed at bioengineering applied to craniofacial morphology.
6.SIMULATORS
6.1 Safe training for safe treatments
SAFE TRAINING, SAFE TREATMENT
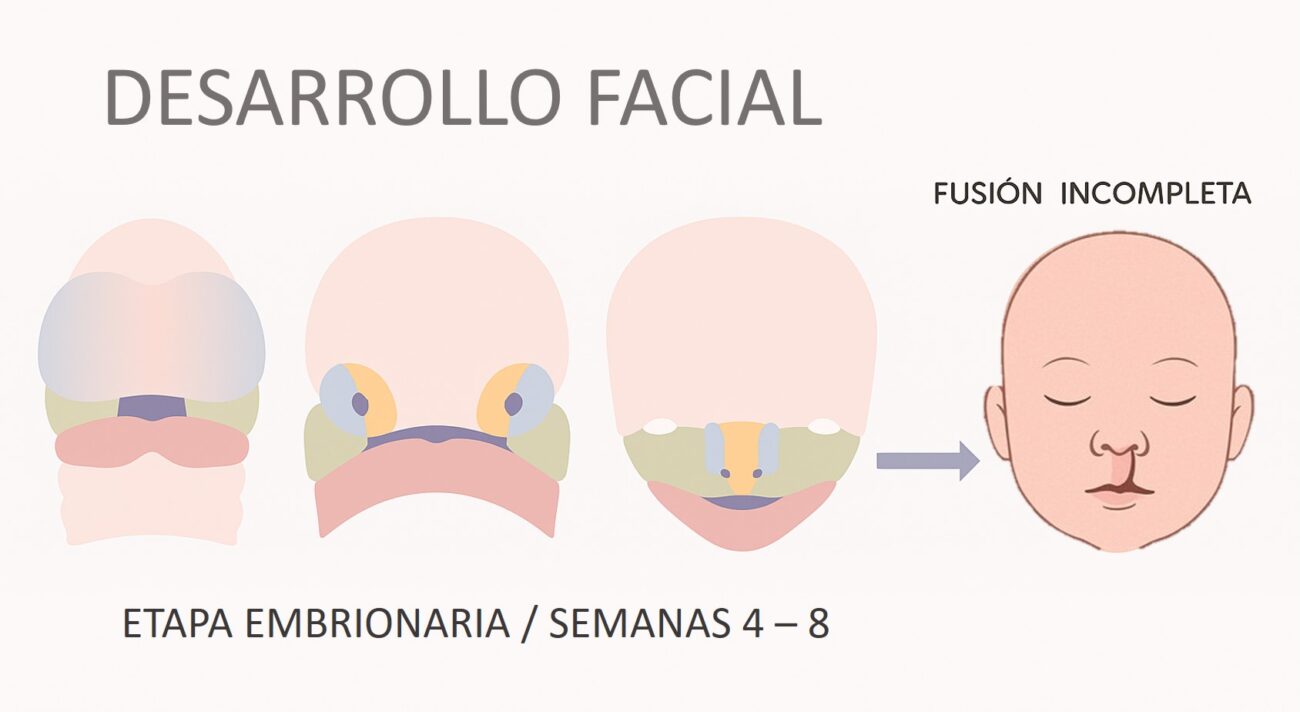
For more than 25 years, my teaching model has focused on providing practical training, rigorous and safe to health professionals who work with infants with cleft lip and palate. One of the most critical stages of the initial approach is the taking intraoral impressions, necessary to start pre-surgical treatment with functional orthopedic devices.
Throughout my years of experience in clinical training with dentists, surgeons and therapists, The need arose to have a teaching tool that realistically simulate the anatomy and behavior of a newborn with cleft lip and palate. This need was the starting point for the design of the Training Simulator, a tool that reproduces the real conditions of a neonate during intraoral impression taking, allowing professionals to train without putting a baby at risk.
6.2 A design oriented towards clinical teaching
The simulator was developed in 2019 with the aim of offering a model that reproduces:
- Las dimensions, weight, facial texture and features of a newborn.
- The intraoral morphology typical of a patient with cleft lip and palate.
- The actual conditions during impression taking with elastic material, with visual and tactile access to the palate and alveolar ridges.
This simulator has become a indispensable tool in the face-to-face courses and clinical workshops that I teach in more than 14 countries, allowing participants to acquire skills with a shorter and safer learning curve.
Beyond technical training
In addition to its pedagogical value for professionals, The simulator has proven to be very useful for educate parents and caregivers. thanks to him, is it possible:
- Show the placement and removal of the Functional Plate in a practical way.
- Teach safe techniques nutrition and oral hygiene of the newborn.
- Build trust in caregivers, by practicing with the model before handling your own baby.
6.3 Why is it still necessary in the digital age?
Although the advancement of digital dentistry has allowed intraoral scanners to gain prominence, clinical reality imposes certain limits:
- The tips of today's intraoral scanners do not yet allow complete access to all regions of the newborn's upper jaw, especially the area of hamular groove.
- Besides, many regions of the world lack access to this technology, Therefore, taking impressions continues to be an essential manual procedure in the care protocol..
For these reasons, the simulator is still a current tool, relevant and effective, especially for the training of professionals in environments with limited resources or in early phases of training.
6.4 Benefits of using the simulator
- Eliminate risks during training: training is carried out in safe conditions, without putting a newborn at risk.
- Improve the learning curve: allows multiple repetitions of the procedure until the necessary technical skill is achieved.
- Higher clinical safety standards: prepares teams to initiate pre-surgical treatments with greater confidence and precision.
- Support for caregivers: educates and reassures families, by allowing them to practice with the simulator before manipulating the baby's oral cavity.
- Teaching versatility: allows you to train different techniques, including the use of nasal elevators, like those proposed by Dr.. Avni Abdi (2019).
The use of the Simulator transforms the way we train professionals who care for the little ones. It is an advance at the service of security, learning and clinical excellence.

7. TRAINING

The Dra. Teresita Pannaci offers programs of training Aimed at health professionals interested in the comprehensive approach to patients with cleft lip and palate and other craniofacial malformations.
Each course combines a solid scientific foundation with the direct clinical application of contemporary Functional Orthopedics of the Jaws techniques. (OFM) and Nasal Molding within the context of presurgical treatment (PSY, Presurgical Infant Orthopedics).
These programs — taught in person or online, individually or in groups—they are designed in a personalized way, guaranteeing a training experience adapted to the profile and objectives of each participant.
One of the most notable features of these training courses is the use of neonatal anatomical simulators., developed by Dr herself. Pannaci, that allow all traditional and contemporary PSIO techniques to be safely taught and practiced before applying them on real patients.
Theoretical-Practical Courses and Workshops
Addressed to:
Dentists specializing in Pediatric Dentistry, Orthodontics and Maxillary Orthopedics, specialists or residents in Maxillofacial Surgery and Plastic Surgery, as well as dental technicians and prosthetists interested in the pre-surgical phase of the treatment of the cleft patient.
General objectives:
The theoretical-practical course offers the conceptual tools and clinical skills necessary to apply the preoperative preparation technique using OFM and Nasal Molding., aimed at the functional rehabilitation of cleft infants.
At the end of the course, The participant will be able to:
- Taking intraoral impressions in neonates with cleft lip and palate.
- Perform jaw molding in pre- and post-surgical phases.
- Rehabilitate vital breathing functions, sucking and swallowing.
- Diagnose and treat patients with Pierre Robin Sequence.
- Perform 2D and 3D dimensional analysis on plaster or digital models to control the treatment sequence.
- Identify and manage errors and complications during the therapeutic process
Course Features:
- Duración: 16 academic hours distributed in 2 a 4 days, according to programming.
- Mode: In person or online.
- Methodology: Conferences, discussion of clinical cases, practical demonstrations and use of simulators.
- Features: Each participant has an individual simulator, practice material and an illustrated manual with the complete sequence of techniques.
Modular structure / Programming
The program is developed in 6 modules distributed in 6 meetings (one per month), with a duration of two days per meeting - Friday and Saturday -.
- The initial modules are dedicated to the treatment of unilateral cases.
- Advanced modules focus on addressing bilateral and complex cases.
Teaching team:
The training is led by Dr.. Teresita Pannaci, accompanied by support instructors specialized in the practical execution of Functional Orthopedics of the Maxillae techniques (OFM) and Nasal Molding.